What is a slipped disc?
The spine is made up of 24 vertebrae. Between the vertebrae lie soft, gel-like discs, which act as a shock-absorber or cushion, absorbing the impact of the spine during daily movements.
According to NHS statistics (2016) a third of UK adults experience low back pain, although only 1 in 20 have slipped a disc. This type of back pain typically affects people aged 30-50, and men are twice as likely to be affected as women.
Usually associated with trauma, the outer-shell of the disc becomes damaged, allowing the gel inside to leak out. The discs lie directly over the spinal nerve root, causing the protruding disc fluid to pressurise the nerve, causing localised back pain. When the nerve is pressed or irritated, people can experience neural symptoms, including numbness, tingling or weakness. Often, the sciatic nerve is compressed, resulting in sciatica or nerve pain into the buttocks, thigh or feet. A slipped, herniated and bulged disc all refer to the same type of injury. The diagnosis indicates the percentage of leaked disc fluid, and whether or not the nerve has been affected.

The red area shows the leaked disc fluid pressing on the spinal nerve (yellow), which can become inflamed, causing back pain and symptoms down the leg.
What causes a slipped disc?
A slipped disc is often associated with trauma or a bending forward motion, although not necessarily. With age, the discs lose some of their water content, making the disc less spongy, and more susceptible to injury following minimal strain. Sometimes twisting or turning whilst lifting heavy objects can cause a sudden sharp back pain. The pain can be specific to the lower back, or cause burning or tingling down the leg. People usually feel pain on one side, however it can be more generalised across the lower back.
Management of a slipped disc
If you have slipped a disc, there are different management options available. Often, the pain improves naturally over time as the disc eventually shrinks away, reducing pressure and relieving pain on the nerve (see Case Study at the bottom of page). This can take 6-8 weeks, or sometimes longer. A combination of pain relief and physiotherapy can usually help to relieve the inflammation, tightness and pain in the back and legs. A Physiotherapist will assess you and use a combination of techniques to speed up healing, reduce pain and increase flexibility. In severe cases, patients can consult an Orthopaedic Surgeon who will advise whether surgical procedures or steroid injections are needed.
Self-management of a slipped disc or low back pain
If you suspect that you have a slipped disc, try to keep mobile and doing your usual activities. If you rest for too long, your joints may stiffen up further, exacerbating your back pain. You may need to take pain killers or anti-inflammatories and rest from the aggravating factors. This will keep your spine flexible, keep your muscles strong and help to speed up healing. Pilates has been shown to effectively manage low back pain, strengthen the core and consequently prevent further injury.
Case Study: The scan below belongs to a 29 year old woman who presented with pain and tingling in her right leg. The patient had a steroid injection, as well as a course of physiotherapy, including massage, stretches and core strengthening. Within five months, her disc herniation had resolved, the pain and paresthesia had gone. (Hong, J & Ball, P (2016) N Engl J Med 2016; 374:1564)
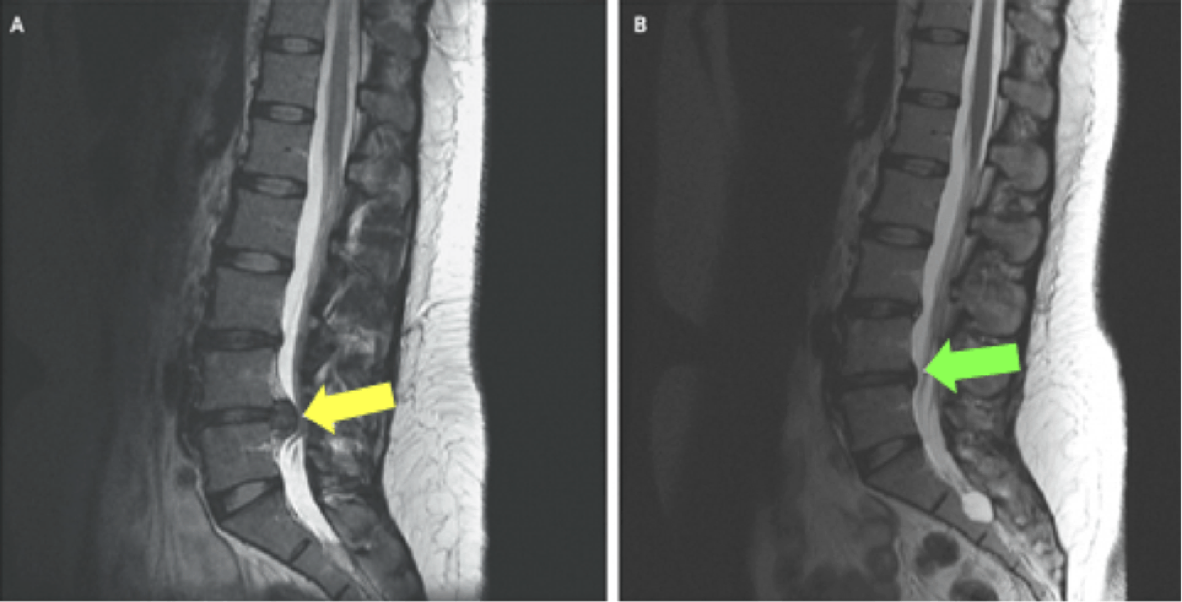
MRI of a lumbar spine showing slipped disc before and after treatment
Figure A: MRI at the time of injury; the yellow arrow shows a lumbar disc herniation and nerve root compression.
Figure B: MRI at 5 months post-injury; the green arrow shows the disc is no longer compressing the nerve or spinal cord (white/grey column next to the vertebrae), with complete resolution of the slipped disc.
If you are worried about your back pain, please contact to discuss how physiotherapy could help you.
Naomi Sofer
Specialist Physiotherapist